Abstract
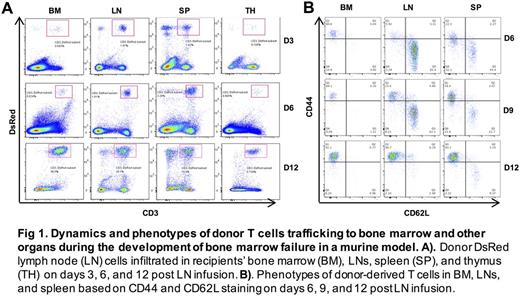
Background and objective T-cell-mediated destruction of bone marrow (BM) hematopoietic stem and progenitor cells (HSPCs) is the pathophysiology of aplastic anemia (AA). Human AA has been modeled in mice by adaptation of historic "runt disease" in which infusion of lymph node (LN) cells into recipients mismatched at MHC or minor histocompatibility (minor-H) antigen loci produced BM failure with severe pancytopenia and marrow hypoplasia that highly resemble manifestations of human AA. These models have been used to test the plausibility of immune mechanisms inferred from the study of patients and patient cells, and also to serve as a platform for testing new treatments. While much has been learned from these models, the dynamics of T cell homing, expansion and localization in target tissues have not been well examined. Thus, we employed C.B10 AA model to characterize T cells trafficking to BM and other organs. Methods C.B10 mice received 5 Gy total body irradiation (TBI) and were then infused with B6-DsRed LN cells at 5×106 cells/mouse via tail vein injection. On days 3, 6, 9, and 12, mice were sacrificed, and BM, spleen, LNs, and thymus were collected to analyze the dynamic change and activation status of donor T cells in these organs by flow cytometry. On day 12, blood was collected from retro-orbital sinus for the analyses of hematologic parameters, while donor-derived (DsRed) T cells were sorted from BM, spleen and LNs into CD3+CD4+ and CD3+CD8+ fractions for RNA isolation and gene expression analyses by PCR array. Results Relative to control animals that received TBI without LN cell infusion, AA mice developed severe BM failure with dramatic decrease in white blood cells, platelets and total BM cells on day 12 after LN cell infusion. Frequencies of DsRed T cells trafficking to BM, LNs and spleen increased with time. Surprisingly there were very few DsRed T cells in BM on days 3 and 6, significantly lower than those in spleen or LNs. On day 12, DsRed T cells increased dramatically in BM to a level much higher than those in the spleen and LNs, suggesting that donor T cells homed primarily to spleen and LNs first, expanded and differentiated, and then trafficked to BM. Frequency of DsRed T cells in thymus was the lowest during the whole process, implying that thymus is more resistant to donor T cell infiltration, which may represent an immune privilege site (Figure 1A). On day 12, CD3+CD8+ and CD3+CD4+ T cells were essentially of donor (DsRed) origin in BM, spleen and LNs of AA mice (CD3+CD8+ at 99.12±0.29%, 92.07±0.90%, and 93.59±1.04%, and CD3+CD4+ at 98.38±0.20%, 82.87±1.81%, and 39.78±4.24%, respectively) except CD3+CD4+ T cells in LNs. Transcriptome analyses showed higher expression in Cd38, Ifng, Lag3, Csf1, Spp1, and Tnfsf13b in BM CD3+CD4+ and CD3+CD8+ T cells, but lower expression in Foxp3 and Ctla4 in BM CD3+CD4+ T cells than did those in spleen and LNs, indicating that BM T cells were at a state with stronger activation but weaker immunosuppression signaling . Meanwhile, we assessed donor T cell phenotypes using CD44 and CD62L markers, and found that almost all donor CD4+ or CD8+ T cells in BM were of effector memory T cell phenotype (EM: CD44+CD62L-) on days 6 , 9 and 12, while T cells in spleen and LNs were of EM, central memory (CM:CD44+CD62L+), and naïve (NA: CD44-CD62L+) phenotypes on days 6 and 9 before converting to EM phenotype on day 12 (Figure 1B), indicating that T cells in the BM were at a more terminal differentiation stage ready for the initiation of HSPC destruction. The expansion of EM T cell phenotype in BM failure mice reflects our recent observation in AA patients from which we found clonal expansion enriched in effector memory CD8+ T cells defined by CD28-CD57+ phenotype (Giudice et al. ASH abstract, 2016). Conclusions We demonstrate here that donor CD3+CD8+ and CD3+CD4+ T cells first home to host spleen and LNs for expansion and differentiation, and then traffick to host BM where they display strong signaling of activation with a terminal effector memory phenotype. The discovery of stage-specific T cell lodging pattern provides fresh insight for the development of new treatment for AA targeting T cell trafficking intervention.
Young: Novartis/GSK to institute: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal